Meniscal tear repair has firmly emerged as the preferred treatment strategy for many knee injuries, marking a decisive shift away from traditional meniscectomy.
With growing evidence linking meniscus preservation to better long-term joint health, recent research highlights how advances in surgical techniques, biologics, and salvage strategies are reshaping outcomes for patients with both simple and complex meniscal tears.
Meniscal injuries affect people across all age groups and remain one of the most common knee pathologies worldwide. Historically, the meniscus was thought to have little functional value, leading surgeons to routinely remove damaged tissue. However, decades of biomechanical and clinical research have demonstrated that the meniscus plays a critical role in load transmission, shock absorption, and joint stability. Total or partial removal has since been associated with early-onset osteoarthritis, joint-space narrowing, and long-term functional decline.
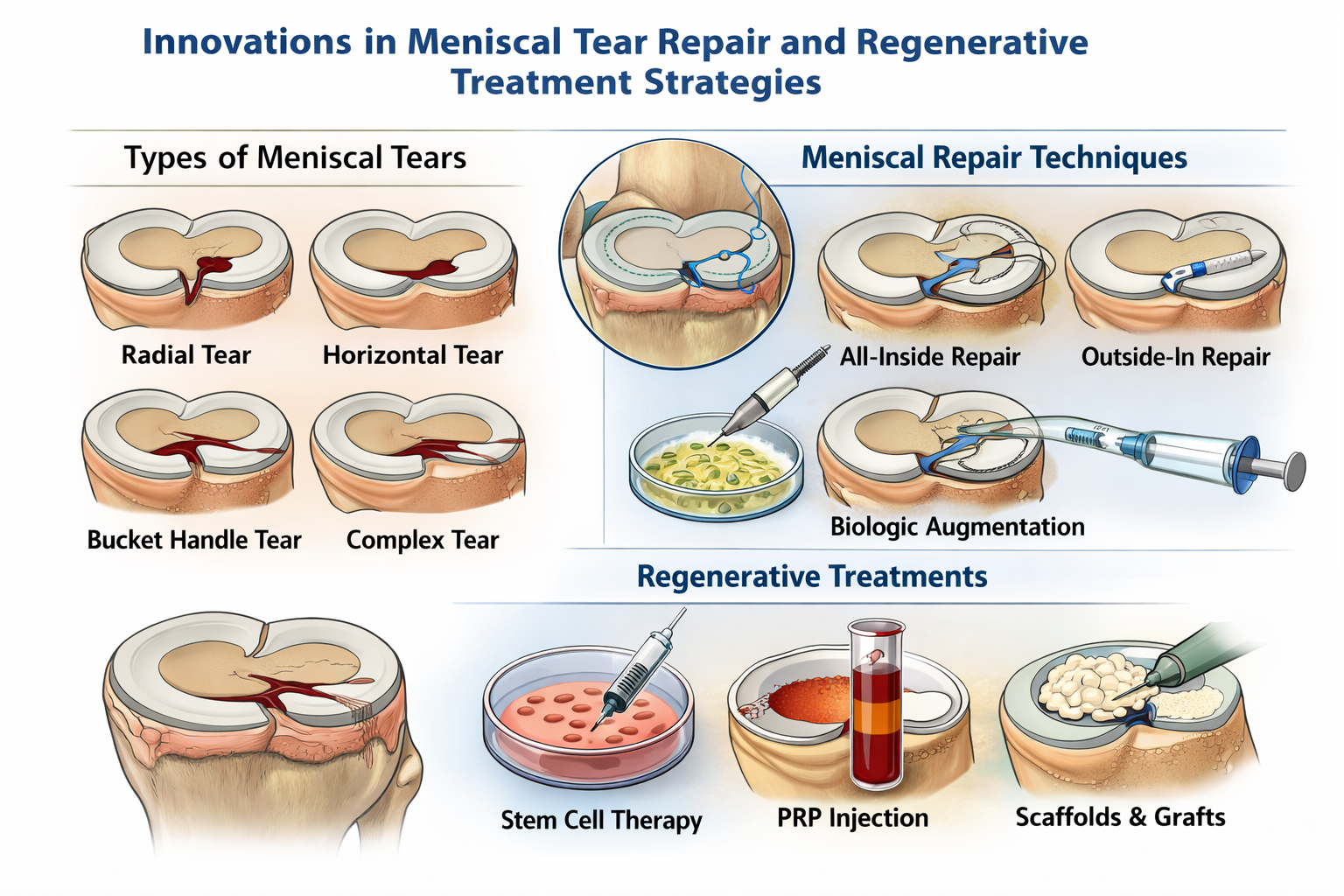
As a result, meniscal repair has become the gold standard whenever feasible. Contemporary repair techniques aim to preserve as much native tissue as possible, particularly in tears located in the vascularized outer regions of the meniscus, where healing potential is higher. Techniques such as inside-out, outside-in, and all-inside arthroscopic repairs are now widely used, with suture-based all-inside devices gradually replacing older rigid implants due to superior biomechanical strength and lower complication rates.
Advances in meniscal repair techniques, biologic augmentation, and salvage strategies are helping surgeons preserve knee function and delay osteoarthritis progression.
Request Sample PDF Report: https://www.quintilereports.com/request-sample/580-meniscal-repair-market/
Despite these advances, not all meniscal tears are easily repairable. Complex, degenerative, radial, or chronic tears—especially those in avascular zones—pose significant challenges. To address these cases, surgeons have increasingly turned to hybrid and salvage techniques. Novel approaches, such as circumferential compression sutures that “pack” unstable meniscal tissue, have shown promising short-term success rates, even in tears previously considered irreparable. Other salvage strategies include rasping tear surfaces, inducing localized bleeding, and using fascia sheaths or exogenous fibrin clots to stimulate healing.
Biologic augmentation has also gained traction as a potential enhancer of meniscal repair outcomes. Platelet-rich plasma (PRP) and stem cell therapies aim to promote tissue regeneration by delivering growth factors that support collagen synthesis, angiogenesis, and cellular repair. While some randomized trials and meta-analyses suggest PRP may reduce repair failure rates and improve pain scores, findings remain inconsistent. Variability in PRP preparation protocols, patient selection, and outcome measures continues to limit definitive conclusions, underscoring the need for standardized, high-quality clinical trials.
For patients with substantial meniscal loss, meniscal scaffolds and allograft transplantation offer alternative solutions. Collagen-based and synthetic scaffolds are designed to support tissue ingrowth and restore meniscal function, while allograft transplantation may benefit carefully selected patients with symptomatic, meniscus-deficient knees. However, these options remain constrained by strict indications, regulatory challenges, cost considerations, and limited long-term evidence.
Postoperative rehabilitation remains a cornerstone of successful meniscal treatment. Protocols emphasize protecting the healing meniscus in the early phase, followed by gradual restoration of range of motion, strength, and functional activity. Rehabilitation timelines differ significantly between meniscal repair and meniscectomy, with repairs requiring more cautious progression to reduce retear risk.
Experts increasingly advocate for personalized treatment algorithms that consider tear type, location, vascular supply, patient age, and activity level. Younger, active patients are more likely to benefit from repair and biologic augmentation, while older individuals with degenerative changes may require alternative approaches.
Meniscal injuries are among the most common orthopedic conditions, affecting individuals across all age groups and activity levels. Earlier surgical approaches favored partial or total meniscectomy, based on the belief that the meniscus served little functional purpose. However, landmark biomechanical and clinical studies revealed that meniscal loss leads to increased joint contact pressures, cartilage degeneration, and a markedly higher risk of early osteoarthritis. These findings prompted a paradigm shift toward meniscal preservation whenever feasible.
Overall, the evolving literature reinforces a clear trend: preserving the meniscus whenever possible leads to superior functional outcomes and improved long-term joint health. While challenges remain—particularly regarding biologics, cost-effectiveness, and surgeon learning curves—the continued refinement of repair and salvage techniques signals a promising future for patients with even the most complex meniscal injuries.
Our Latest Publication
Meniscal Repair Market Size Estimation, Share & Future Growth Trends Analysis, By Product (Suture Meniscal Repair, Implant Meniscal Repair, Hybrid Meniscal Repair), By Application, By End Use, and Regional Analysis, 2024-2032
Adarsh
Business Strategy — Quintile Reports
Adarsh is a Business Strategy professional focused on transforming market insights into actionable growth plans. He supports strategic initiatives through market analysis, competitive intelligence, and data-driven decision-making to help drive long-term business success.
His core skills include strategic planning, market research, growth opportunity assessment, trend analysis, performance tracking, stakeholder communication, cross-functional collaboration, and critical problem-solving.